Mechanisms of AMR: Mdr Genes and Antibiotics Decoys Retard the New Antibiotic Discovery against Superbugs-Juniper Publishers
Novel Approaches in Drug Designing & Development (NAPDD)
Many microorganisms cause lethal diseases in human
causing loss of lives and property worldwide. Many antibiotics are used
to cure deadly infections for the past 75 years with no difficulty.
Recent outbreaks of multi-drug resistant bacteria have caused millions
of death every year and physicians do not know how to cure KPC2 Klebsiella kneumoniae, NDM1 Escherichia coli or MRSA Staphylococcus aureus and XDR Acinetobacter baumannii
infections. Sadly once used ampicillin, streptomycin, azithromycin,
tetracycline, and chlormphenicol are useless against those bacteria.
Combination therapy using colistin, imipenem, amakacin, ceftizidime and
investigation drug ovibactam sometime are giving good clinical efficacy
but not sure. In such a situation, heterogeneous phyto-antibiotics and
gene medicines have been welcome by medical authorities but AMR calamity
remains as mdr genes (amp, bla, tet, cat, aac, aad, aph,sul etc) moved to conjugative plasmids and chromosome of bacteria with target specific alterations in rRNA and porins genes.
Keywords: Mdr genes; Anti-microbial resistant; Gene medicine; Phyto-antibiotics Introduction
Past 75 years are the golden era of drug development
and several types of antibiotics are in centre stage of such discoveries
since the discovery of penicillin drug by Alexander Flaming from slime
mold Penicillium notatam in 1928 targeting peptidoglycan cell wall
biosynthesis of most Gram (+) and Gram (-) bacteria [1].
Since then 1000 derivatives were made alone for penicillins
(ampicillin, cefotaxime and imipenem) for better drug usually called
penicillinases resistant drug. A professor of biochemistry and
microbiology at Rutgers University, Dr. Selman A. Waksman discovered
over twenty antibiotics (a word he coined) and introduced procedures of
antibiotic production (streptomycin) that led to Nobel Prize in
Physiology or Medicine in 1952. However, such dream could not last long
as more potent penicillinases called, oxacillinases, cefotaximases,
carbapenemases were appeared in bacterial plasmids [2].
New era of biology was begun in 1953 with the
discovery of structure of DNA, gene structure, regulation of gene
expression and advancement of DNA sequencing, chromosomal structure and
RDT work (Figure 1).
Profound impact was found by biomolecules separation by ultra
centrifugation and HPLC with chemical structure analysis by Mass, NMR
and FTIR. Invitebly we got many life saving drugs with known target site
although basic DNA, RNA and protein composition in virus to bacteria to
human were same [3].

Semi-synthetic drugs and anti-microbial resistance
Naturally, semi-synthetic drugs were made without choice to overcome the action of multi-drug resistant class
located in bacterial plasmids that inactivate the antibiotics by
different mode of actions. As for example, ampR cell extract was
discovered as early as 1940 and amp gene which produces an enzyme, Beta-
lactamase was sequenced in 1965. Now one in three bacteria in river and
sea water contained amp gene in large conjugative plasmids that also
carry 5-10 other mdr genes and 10-15 Tra and Tnp genes [4].
So journey from 1940-1960, described the isolation of tetracycline,
streptomycin, sulfa-drug, ampicillin, amoxicillin, cefoxitin,
cefotaxime, erythromycin, nalidixic acid, ciprofloxacin, neomycin,
polymyxin, enoxacin, norfloxacin (Figure 2).
However, at the almost same time, resistant bacteria to all these
antibiotics were developed creating pressure to drug industry for more
and more new drug development. However, it is not very easy to develop a
drug for human use because it needed at least one billion dollar to
develop a drug. What happen to investor if a developed drug is good for
few years and then drug resistant microbes appeared when no one want to
prescribe that antibiotic because uncertainty of cure of such infections
and also delay in treatment and also taken of repeated different
antibiotics surely toxic to health and time and monetary loss [5].

Drug screening from bacteria against bacteria-a wrong message
In fact, now R & D Industry screening new drugs
everyday and also computer-guided graphics design and stimulate
artificial drug-target interactions have accelerating the new drug
development. Screening of new drug from fungi was favourable in sense
that in soil and water there is a battle between bacteria and fungi and
so fungi will produce anti-bacterial to kill bacteria. That type of
selection is good having different genus but what we did that we
introduced the battle between actinomycetes and bacteria like neomycin
(1946) and actinomycin (1940). And then we introduced the battle between
bacteria against bacteria as for example streptomycin is produced from
soil bacteria, Streptomyces griseus and also chloramphenicol that
eradicate typhoid disease in early decades. What has happened in life
of bacteria that all want to destroy it and as a result bacteria are
forced to re-arrange its genes to save its life, Hypothesis is not so
easy as its own counterpart is enemy and bacteria created many new
entity like transposons, integrons, R-plasmids and many DNA
rearrangement enzymes like transposes, resolves and integrases and also
many topoisomerases and restriction end nucleases [6].
In 1960-1980, we produced 1000 tons of antibiotics in industry and 7000
millions of global peoples now taken antibiotics almost every day or
every month to remove the bacteria from intestine and blood to keep
healthy. Doctors have forgotten that bacteria needed for human
development and intestine should stay (10)12 bacteria for normal
synthesis of vitamins which human could not synthesize itself . When
such discrepancy was noticed, then probiotic bacteria were used as
supplement after each antibiotic therapy. In other word, we used many
unnecessary doses of antibiotics as for example, for viral infection,
for pain and in food animal growth as well as in agricultural land [7].
Conjugation plasmid-a safe guard of bacteria to transmit genes without failure
However that is too late, as bacteria developed
another armour against antibiotics by using its very urgent plasmids
used in conjugation (marriage) that means bacteria could form a sex
pilus using Tra proteins coded by 62kb plasmid called F'- plasmid which
usually did not carry MDR genes. What bacteria did that combined
R-plasmid with F'-plasmid and such plasmid is known today as conjugative
MDR plasmid which could be large as 100-500kb and such plasmids are
hard to purify by plasmid purification method for molecular biological
study being contaminated with bacteria chromosome (2000-5000kb) [8].
Never the less CsCl density gradient centrifugation and Pulse Field Gel
Electrophoresis have help to isolate such plasmids with purity and also
fully sequenced. What we see that such plasmids carry most Tra and Tnp
genes including localized mdr genes. What is the advantage of bacteria
then? Very advantage for life because such plasmids are very stable in
bacteria during cell division and also could donate the non-MDR bacteria
of mdr genes to save from deleterious effects of antibiotics and toxic
chemicals in water. What is a toxic chemical? Well large industry like
mineral Industry, Paint industry, drug industry, paper industry,
petroleum industry and excreta from 100 million peoples in many big
cities (New York) releases tons of chemicals, antibiotics and heavy
metals into sea water that are very harmful to bacterial central dogma
enzymes like those involved in replication, transcription and
translation. What exactly bacteria did Bacteria simply made 100
different enzymes that destroy antibiotics once it entered into
bacteria. But that is not sure as 100 chemicals and detergent in sewage
water and bacteria made drug efflux genes (known as tetA, acrAB,
mexAB/CD/EF, and ABC genes) that could remove drugs and chemicals from
cytoplasm into outside keeping save its cellular enzymes and nucleic
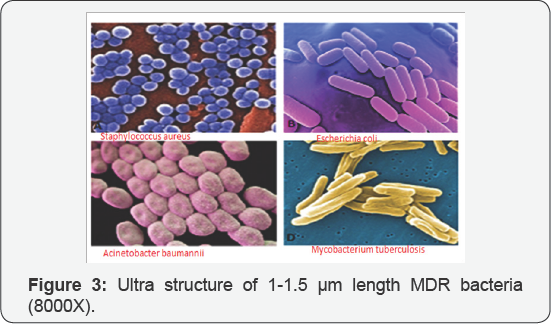
acids (Figure 3).
That mean whatever the high concentration of pollutants and antibiotics
outside water where bacteria live no toxicity because once a chemical
enter into bacteria acrAB/C proteins pump it back into environment
keeping bacteria safe. What is the consequence? Well bacteria in our
body stay alive and divide most to cause sepsis and trauma but condition
not likely going to improve by taking prescription drugs because no
achievable concentration of the drug would be happen in bacterial
cytoplasm (to stop protein synthesis) due to bacterial drug efflux pumps
(Figure 4).

Bacteria moved mdr genes into chromosome to increase gene dose further
Did any other genetic changes happen that we should
be worry? Yes, bacteria also made safe guard by combing mdr genes into
their chromosome and few bacteria like Staphylococus aureus and Acinetobacter baumannii and also household bacteria like Escherichia coli genome-MDR-islands were sequenced confirming the calamity (Figure 4).
That is not the end, porin membrane proteins are also mutated in such a
way that antibiotics receptors altered and no drug could enter into
bacteria at low drug concentration giving MDR. Further, ribosomal
ribonucleic acids (23S, 16S rRNAs) gathered few mutations (usually very
conserved) and many ribosomal proteins and drugs interactions did
altered causing MDR. On one word, bacteria have achieved many shrouds
against antibiotics and drug companies did not know where to start [9].
As for example, we discovered at least twenty types'
bacterial beta-lactamases (mdr genes) that were sequenced. Again in each
type beta-lactamase gene, hundreds of mutations were discovered that
sometime gave high drug resistance increasing drug MIC or totally
resistant. Gen Bank analysis clearly showed that each conjugative
plasmid in Pseudomonas aeruginosa, Klebsiella kneumoniae, Escherichia coli and Salmonella typhi have many mdr genes giving resistant to 5-10 antibiotics from different groups with different mode of ations (Table 1).
Interestingly such plasmids carry mdr genes in one locus with
activation by transposon promoter-enhancers and Tra genes are located in
clusters (Figure 5).
It is very easy to isolate MDR bacteria in water by adding antibiotics
in media at 50μg/ml and then isolate plasmid DNA by alkaline lyses
method and then do PCR reactions in presence of mar gene specific
primers as shown (Figure 6) where Escherichia coli
KT-1_mdr bacterial plasmids were amplified with mcr, tet, bla VIM and
acrAB mdr genes specific primers. Such PCR product could be confirmed by
di- deoxy DNA sequencing as shown in (Figure 7) where blaTEM gene was found in every ampicillin resistant bacteria we have isolated from Ganga River water of Kolkata [3,10].




Conclusion
It is very evident that superbugs were highly
contaminated in water resources of India similar to other Asian and
American countries [11,12].
WHO warned that if alternative to antibiotics were not discovered, very
fatal human loss might be occurring in the future? Likely herbal
antibiotics research has given priority in India as there is enough
medicinal plants and spices available as described in Sanskrit books
Charaka Samhita and Veda [8].
However, gene medicines (ribozymes, miRNA, antisencse RNA, and DNA
nanotechnology have benn welcome to stop the horror of MDR bacterial
pathogenesis. MDR phenomenon is ancient and also universally have
detected in viral pathogenesis, cancer cells and parasitic diseases [13,14].
More sadly, bacteria have acquired promoter induction system by
antibiotics and many transcription factor repressors (tetR, acrR) have
been accumulated in conjugative plasmid. What it mean that if you take
imipenem then it will activate MDR genes causing more AMR and simply
patient will die on antibiotic treatment [15].


Comments
Post a Comment